ISC 12>STRUCTURE AND FUNCTION OF ANIMALS>3. RESPIRATORY SYSTEM
SCOPE OF SYLLABUS
Organs involved in respiration;
mechanism of pulmonary gas exchange;
breathing process should be explained showing the action of diaphragm and intercostal muscles,
regulation of respiration;
transport of oxygen in the blood, oxyhaemoglobin dissociation curve;
transport of CO2; chloride shift,
disorders of respiratory system such as - asthma, emphysema, occupational respiratory disorders.
mechanism of pulmonary gas exchange;
breathing process should be explained showing the action of diaphragm and intercostal muscles,
regulation of respiration;
transport of oxygen in the blood, oxyhaemoglobin dissociation curve;
transport of CO2; chloride shift,
disorders of respiratory system such as - asthma, emphysema, occupational respiratory disorders.
Model of respiratory system
Respiration and types of respiration
|
The process by which food is oxidized in the cells to release their bond energy for utilization in the body is known as respiration.
Depending on the availability of oxygen, respiration is classified as Aerobic – with oxygen Complete oxidation of carbohydrates producing carbon di oxide, water and energy. Anaerobic – without oxygenIncomplete degradation of substances and release of carbon di oxide, organic compounds like ethyl alcohol, lactic acid etc. and energy. |
Respiration in aerobic animals
|
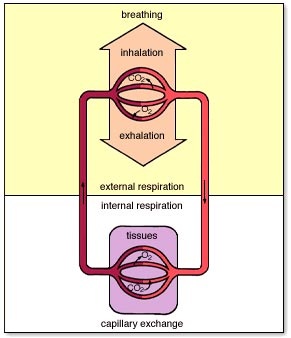
The process of respiration involves two phases- External and Internal respiration.
External respiration involves uptake of oxygen from the environment and elimination of carbon di oxide in the same medium. This is a physical process that depends upon the principle of diffusion. Internal respiration is a physico – chemical process in which energy is produced. Internal respiration involves oxygen uptake by the tissues, oxidation by enzymes and carbon di oxide elimination from the tissue cells. |
RESPIRATORY EXCHANGE
The exchange of gases between the cells and the extracellular fluid and also between animal and the surrounding is based on the principle of diffusion.Gas diffuses across a membrane from the side where its partial pressure is higher to the side where its partial pressure is lower.
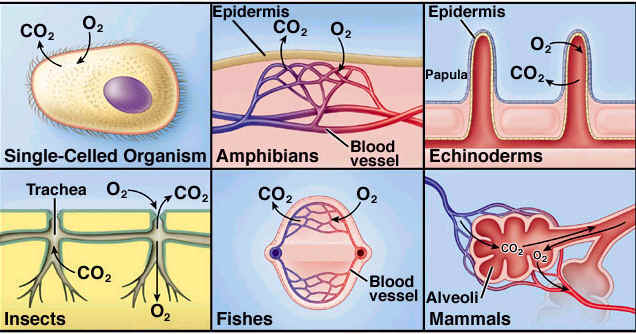
Respiratory surface
|
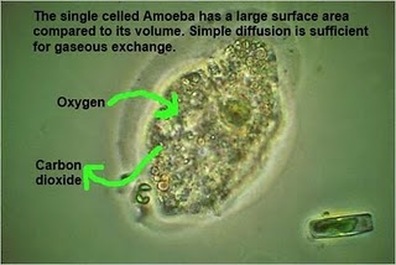
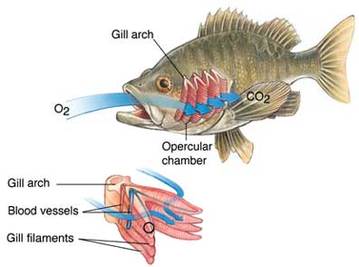
A respiratory surface is needed, with large surface area, thin, highly vascular, permeable to respiratory gases etc.
To meet all these needs complex respiratory systems have evolved. Direct and indirect respiration: Lower animals take the gases directly from the medium and give out to the medium this is called direct respiration. The higher organisms require respiratory and circulatory system, thus is referred to as indirect respiration. |
Respiratory surface in different animals
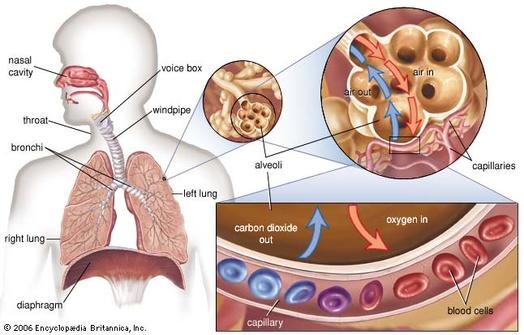
HUMAN RESPIRATORY SYSTEM
Two main components of the respiratory system
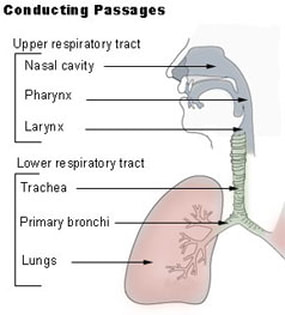
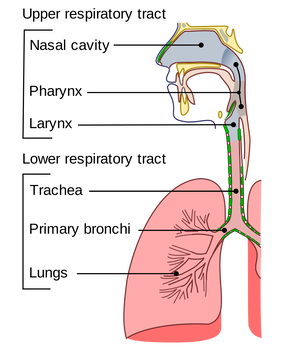
RESPIRATORY TRACT- conducting passage and the respiratory passage
RESPIRATORY ORGAN - Lung
RESPIRATORY TRACT- conducting passage and the respiratory passage
RESPIRATORY ORGAN - Lung
Human respiratory tract
The parts of the respiratory tract
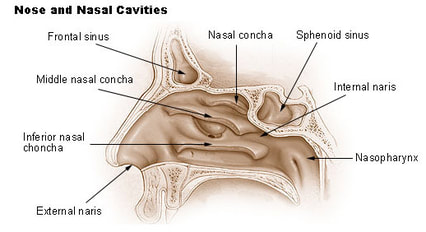
Functions of the nasal passage
1. Passage for air- for going to and from lungs
2. Filtration- Hairs trap large dust particles and mucus traps small dust particles.
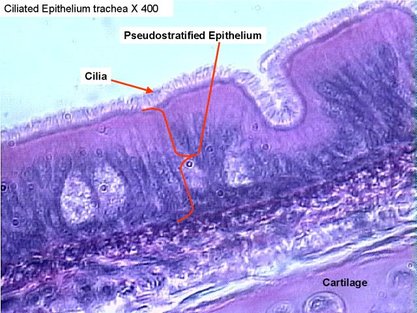
3. Cleaning- cilia vibrate in opposite direction to inhaled air and keeps the passage clean.
4. warming- the blood supply warms or cools the air to bring it to body temperature before entering the lungs.
5. Smell- olfactory receptors detect smell.
6. Sterilisation- Adenoid cells of pharyngeal tonsils kill bacteria.
2. Filtration- Hairs trap large dust particles and mucus traps small dust particles.
3. Cleaning- cilia vibrate in opposite direction to inhaled air and keeps the passage clean.
4. warming- the blood supply warms or cools the air to bring it to body temperature before entering the lungs.
5. Smell- olfactory receptors detect smell.
6. Sterilisation- Adenoid cells of pharyngeal tonsils kill bacteria.
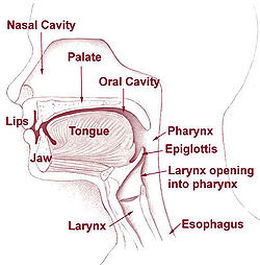
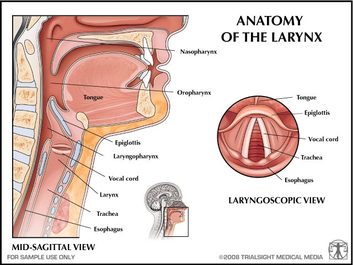
Pharynx and Larynx
|
The opening of the pharynx into the trachea is called glottis and is guarded by cartilaginous flap the epiglottis. During swallowing the epiglottis closes glottis and keeps food out of the respiratory tube.
|
It is the upper part of the trachea, formed of four cartilages, two sets of muscles and two pairs of vocal cords. The vibrations of the vocal cords produces voice.
|
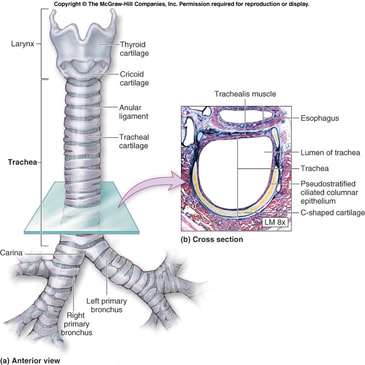
Trachea
|
Trachea extends from the larynx to the bronchi in the thoracic cavity.
It is 11 cm long and 2.5 cm in diameter. The trachea is supported by C- shaped cartilagenous rings. These prevent the collapsing of the trachea. The trachea bronchi and bronchioles are lined by glandular and pseudostratified columnar epithelium containing ciliated and goblet cells.
The goblet cells secrete mucus- it keeps the trachea moist and entangles dust particles that enter with inspired air. The cilia push them upward into the pharynx. The terminal and respiratory bronchiole lack goblet cells. |
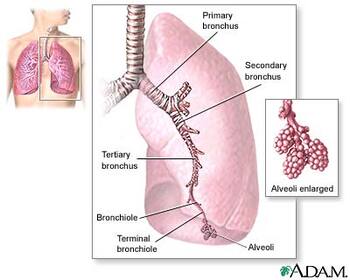
Bronchi and Bronchioles
The trachea divides into two primary bronchi, that enters the lung and divides into secondary and tertiary bronchi.The trachea, bronchi and terminal bronchioles form the conducting zone. These branch into bronchioles- terminal and respiratory. The respiratory bronchioles are without cartilaginous rings. The respiratory bronchioles, alveolar duct and the alveoli form the respiratory zone.
Each respiratory bronchiole divides into a number of alveolar ducts that further divide into atria, which swell up into alveoli or air sacs
The bronchus with its branches is called as the bronchial tree.
Each respiratory bronchiole divides into a number of alveolar ducts that further divide into atria, which swell up into alveoli or air sacs
The bronchus with its branches is called as the bronchial tree.
The bronchi enter into right and left lungs of either side. Inside the lungs they further branch into many smaller bronchioles with a diameter of about 1 mm. These further divide into terminal and then into respiratory bronchioles. Each respiratory bronchiole divides into a number of alveolar ducts that further divide into atria, which swell up into alveoli or air sacs
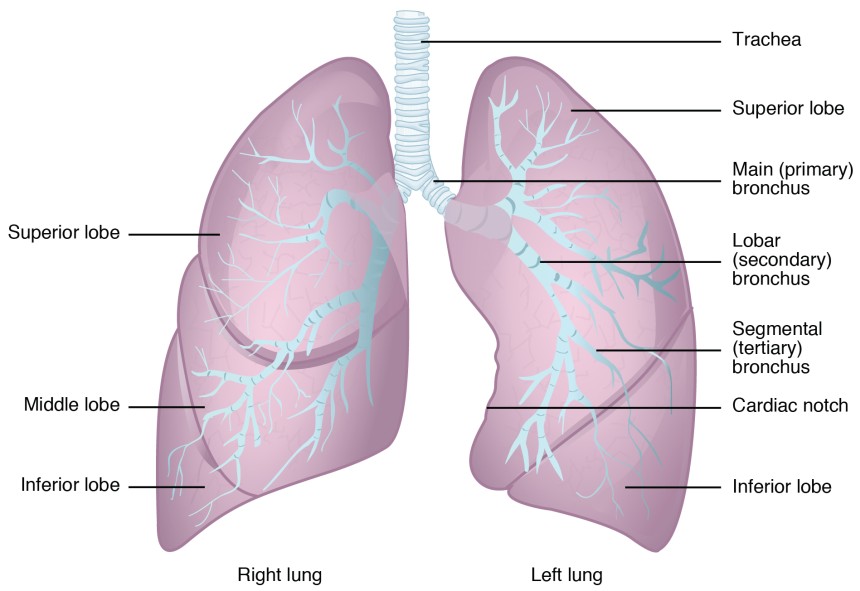
Lung and its membrane
|
Lungs are the principal organs of respiration. These are a pair of sub-conical, elastic hollow bag-like organs with a narrow apex and broad base. It has a broad concave semilunar base to accommodate the diaphragm.
They are located on either side inside the thoracic cavity. The slit through which the bronchus enters is called hilum. The right lung is larger and has three lobes whereas the left lung is smaller and has only two lobes. Left lung has a cardiac notch to accommodate the heart. |
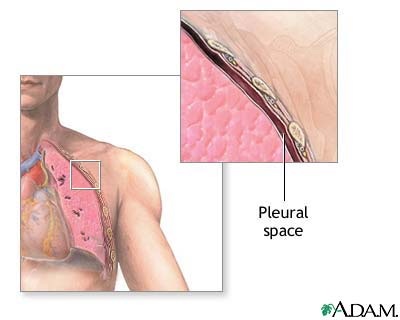
The lungs are enclosed by a double layered membrane called pleura. The membranes are separated by thin space filled with pleural fluid. The membrane that covers the lungs is called viseral pleura and the membrane lining the cavity is called parietal pleura.
Pleural fluid provides frictionless movement to the lungs, and acts as shock absorber. |
WHAT HAPPENS IF WE BREATHE IN PURE OXYGEN? FIND OUT
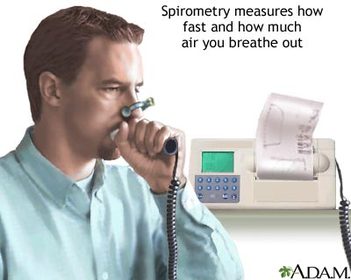
Spirometer and spirogram
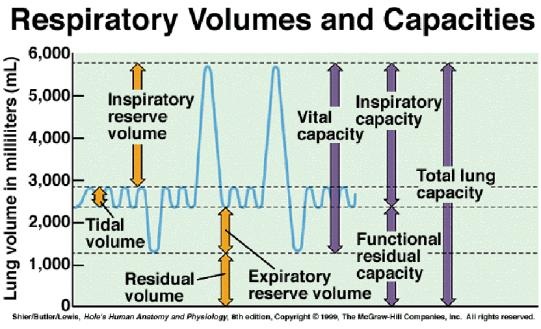
Lung volumes
- Tidal volume- 500ml is the amount of air that can be inhaled and exhaled during one normal (quiet) breathing cycle (about 500 ml for men & women).
- Inspiratory reserve volume (IRV)- 2000-3000 ml - is the amount of air that can be forcibly inhaled beyond a tidal inhalation (about 3,000 ml for men & 2,000 ml for women).
- Expiratory reserve volume (ERV)- 1000-1500 ml- is the amount of air that can be forcibly exhaled beyond a tidal exhalation (about 1200 ml for men & 700 ml for women)
- Vital capacity- 4500ml - TV + IRV + ERV.
- Residual volume- 1500ml - the amount of air remaining in the lungs after an ERV (= about 1,200 ml in men & women).
- Functional residual volume (FRV)- 2500 ml- is the volume of air present in the lungs at the end of passive expiration.
- Total lung capacity- 5000-6000 ml- RV + VC.
Pulmonary respiration
This involves-
1. Ventilation or breathing.
2. Exchange of gases on the alveolar surface or external respiration.
3. Transport of gases.
4. Exchange of gases in the tissues or internal respiration.
1. Ventilation or breathing.
2. Exchange of gases on the alveolar surface or external respiration.
3. Transport of gases.
4. Exchange of gases in the tissues or internal respiration.
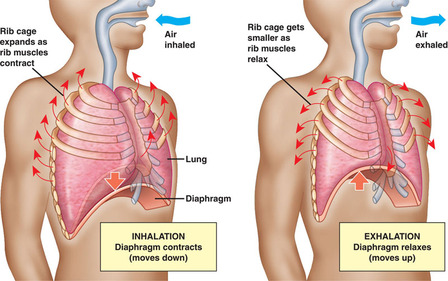
1.Ventilation or breathing-
Involves letting in fresh air into the lungs and CO2 out of the lungs. The intake of fresh air is called Inspiration or inhalation and the elimination of deoxygenated air is called expiration of exhalation.RESPIRATORY CYCLE
One inspiration and one expiration alternately is called respiratory cycle.
Rate of respiration is expressed in terms of ventilation rate. Average- 12 to 14 times.
One inspiration and one expiration alternately is called respiratory cycle.
Rate of respiration is expressed in terms of ventilation rate. Average- 12 to 14 times.
INSPIRATION
|
EXPIRATION
|
Competitive focus: respiratory centers
Breathing is controlled by a poorly defined group of neurons in the brain stem called the respiratory center. The components of this center are widely scattered throughout the pons and medulla oblongata. However, two areas of the respiratory center are of special interest. They are the rhythmicity area of the medulla and the pneumotaxic area of the pons.
The medullary rhythmicity area includes two groups of neurons that extend the length of the medulla. They are called the dorsal respiratory group and the ventral respiratory group.
The dorsal respiratory group is responsible for the basic rhythm of breathing. The neurons of this group emit bursts of impulses that signal the diaphragm and other inspiratory muscles to contract.
The impulses of each burst begin weakly, increase in strength for about two seconds, and cease abruptly. The breathing muscles that contract in response to the impulses cause the volume of air entering the lungs to increase steadily. The neurons remain inactive while expiration occurs passively, and then they emit another burst of inspiratory impulses so that the inspiration-expiration cycle is repeated.
The ventral respiratory group is quiescent during normal breathing. However, when more forceful breathing is necessary, the neurons in this group generate impulses that increase inspiratory movements.
The medullary rhythmicity area includes two groups of neurons that extend the length of the medulla. They are called the dorsal respiratory group and the ventral respiratory group.
The dorsal respiratory group is responsible for the basic rhythm of breathing. The neurons of this group emit bursts of impulses that signal the diaphragm and other inspiratory muscles to contract.
The impulses of each burst begin weakly, increase in strength for about two seconds, and cease abruptly. The breathing muscles that contract in response to the impulses cause the volume of air entering the lungs to increase steadily. The neurons remain inactive while expiration occurs passively, and then they emit another burst of inspiratory impulses so that the inspiration-expiration cycle is repeated.
The ventral respiratory group is quiescent during normal breathing. However, when more forceful breathing is necessary, the neurons in this group generate impulses that increase inspiratory movements.
Factors Affecting Breathing
There are chemosensistive areas within the respiratory center. These areas are located in the ventral portion of the medulla oblongata near the origins of the vagus nerves. They are very sensitive to changes in the blood concentrations of carbon dioxide and hydrogen ions. Thus, if the concentration of carbon dioxide or hydrogen ion rises, the chemosensitive areas signal the respiratory center, and the rate and depth of breathing are increased. Then, as a result of increase breathing rate, more carbon dioxide is lost in exhaled air, the blood concentrations of these substances are reduced, and the breathing rate decreases.
Low blood oxygen seems to have little direct effect on the chemosensitive areas associated with the respiratory center. Instead, changes in the blood oxygen concentration are sensed by chemoreceptors in specialized structures called the carotid and aortic bodies, which are located in walls of certain large arteries (the carotid arteries and the aorta) in the neck and thorax. When these receptors are stimulated, impulses are transmitted to the respiratory center, and the breathing rate is increased. However, this mechanism is usually not triggered until the blood oxygen concentration reaches a very low level; thus, oxygen seems to play only a minor role in the control of normal respiration.
An inflation reflex helps to regulate the depth of breathing. This reflex occurs when stretch receptors in the visceral pleura, bronchioles, and alveoli are stimulated as result of lung tissues being overstretched. The sensory impulses of this reflex travel via the vagus nerves to the pneumotaxic area of the respiratory center and cause the duration of inspiratory movements to shorten. This action prevents over inflation of the lungs during forceful breathing.
http://www.physioweb.org/respiration/control_breath.html
Low blood oxygen seems to have little direct effect on the chemosensitive areas associated with the respiratory center. Instead, changes in the blood oxygen concentration are sensed by chemoreceptors in specialized structures called the carotid and aortic bodies, which are located in walls of certain large arteries (the carotid arteries and the aorta) in the neck and thorax. When these receptors are stimulated, impulses are transmitted to the respiratory center, and the breathing rate is increased. However, this mechanism is usually not triggered until the blood oxygen concentration reaches a very low level; thus, oxygen seems to play only a minor role in the control of normal respiration.
An inflation reflex helps to regulate the depth of breathing. This reflex occurs when stretch receptors in the visceral pleura, bronchioles, and alveoli are stimulated as result of lung tissues being overstretched. The sensory impulses of this reflex travel via the vagus nerves to the pneumotaxic area of the respiratory center and cause the duration of inspiratory movements to shorten. This action prevents over inflation of the lungs during forceful breathing.
http://www.physioweb.org/respiration/control_breath.html
2.External respiratory exchange
|
The partial pressure of oxygen in alveolar air is 100 mm Hg and that of blood is 40 mm Hg.
Due to this difference in partial pressures oxygen diffuses from the lung to the capillaries. The pulmonary veins that collect this oxygenated blood has Poxygen of 95 mm Hg. The P carbon di oxide in the alveoli is 40mm Hg whereas that of the capillaries have 46 mm Hg. Due to this difference, carbon di oxide diffuses from capillaries to the alveoli. A gradient is present for CO2 from tissues to blood and blood to alveoli. As the solubility of CO2 is 20-25 times higher than that of O2, the amount of CO2 that can diffuse through the diffusion membrane per unit difference in partial pressure is much higher compared to that of O2. |
|
THE ADAPTATION OF ALVEOLUS AND GAS EXCHANGE
|
The diffusion membrane is made up of three major layers,
the thin squamous epithelium of alveoli, the endothelium of alveolar capillaries and the basement substance in between them. This allows easy diffusion of gases with only a short distance for diffusion. There is a rich capillary network surrounding the alveolus, that allows gases to move from blood to alveolus and alveolus to blood. The inner surface of the alveolus is moist, this facilitates easy diffusion of gases and prevents the sides of the alveolus from sticking to each other. However, its total thickness is much less than a millimetre. Therefore, all the factors in our body are favourable for diffusion of O2 from alveoli to tissues and that of CO2 from tissues to alveoli. |
3. Transport of gases
|
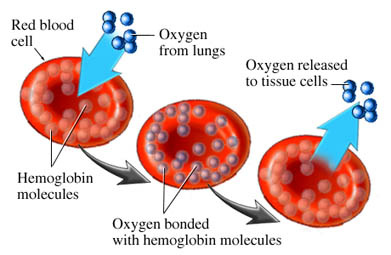
Transport of oxygen
1. Dissolved in the plasma. This accounts for very less amounts of oxygen. 2. As Oxyhaemoglobin: oxygen diffuses into the RBC and combines with Fe ions of Haemoglobin to form oxyhaemoglobin. Factors affecting affinity of Hb for oxygen The pH of blood The temperature BOHR effect: The decrease in O2 affinity of Hb when the pH of blood falls is called the Bohr effect. |
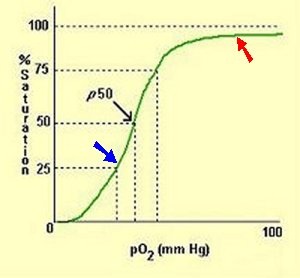
Oxygen dissociation curve
The amount of oxygen that can bind with Hb is determined by O2 tension.
Percentage of Hb that is bound with O2 is called percent saturation of Hb.
This percentage saturation of Hb with O2 is expressed graphically by a curve called the O2-Hb dissociation curve or O2 dissociation curve.
This is sigmoid in shape.
Percentage of Hb that is bound with O2 is called percent saturation of Hb.
This percentage saturation of Hb with O2 is expressed graphically by a curve called the O2-Hb dissociation curve or O2 dissociation curve.
This is sigmoid in shape.
Transport of Carbon di oxide
Carbon di oxide is transported in three forms:
1. As simple solution dissolved in the plasma.
2. As bicarbonate – CO2 reacts with water to form carbonic acid, catalysed by carbonate anhydrase.
Carbonic acid dissociates into bicarbonates and hydrogen ions.
Hydrogen ions are picked up by proteins, some of the bicarbonate ions remain in the RBC whereas some comes out in the plasma. Chloride ions move in, this is called chloride shift or Hamburger shift.
3. As carbaminohaemoglobin about 30% CO2 loosely combines with the globin part of deoxyhaemoglobin
Carbon di oxide is transported in three forms:
1. As simple solution dissolved in the plasma.
2. As bicarbonate – CO2 reacts with water to form carbonic acid, catalysed by carbonate anhydrase.
Carbonic acid dissociates into bicarbonates and hydrogen ions.
Hydrogen ions are picked up by proteins, some of the bicarbonate ions remain in the RBC whereas some comes out in the plasma. Chloride ions move in, this is called chloride shift or Hamburger shift.
3. As carbaminohaemoglobin about 30% CO2 loosely combines with the globin part of deoxyhaemoglobin
4. Internal respiratory exchange
|
Release of CO2 in lung
When deoxygenated blood reaches, the lung there is a difference in partial pressure of the CO2 in the lungs and the capillaries. A series of reactions also takes place as Hb takes up O2, the bicarbonate reacts with H+ and forms carbonic acid, which splits into CO2 and water. Haldane effect Binding of O2 with Hb tends to displace CO2 from the blood. This effect is called Haldane effect. Haldane effect results from the fact that combination of O2 with Hb causes Hb to be a stronger acid. Thus displaces CO2. |
RESPIRATORY DISORDERS
|
Your browser does not support viewing this document. Click here to download the document.
|
|